
 International Glaucoma Week 2016 was observed at The UWI’s Optometry Unit of the Faculty of Medical Sciences, by mainly the second- and third-year students performing ocular screening on members of the public. This was coordinated by Dr. Subash Sharma, the Clinical Coordinator with help from other members of the Unit. International Glaucoma Week 2016 was observed at The UWI’s Optometry Unit of the Faculty of Medical Sciences, by mainly the second- and third-year students performing ocular screening on members of the public. This was coordinated by Dr. Subash Sharma, the Clinical Coordinator with help from other members of the Unit.
This is a comment on the method, patient numbers, enthusiasm of the students and some insights into the results. This is the third time we have observed Glaucoma Week, but the previous two occasions were very low-profile attempts due to equipment insufficiency, busy staff and students who were not full appraised of the importance of the situation. After this resounding success the occasion will definitely be an annual occasion to be observed in our calendar.
The time allotted to the screening was two hours per day, with a final four-hour outreach screening session at the Health Services Unit at the St. Augustine Campus, which was overrun by numbers!
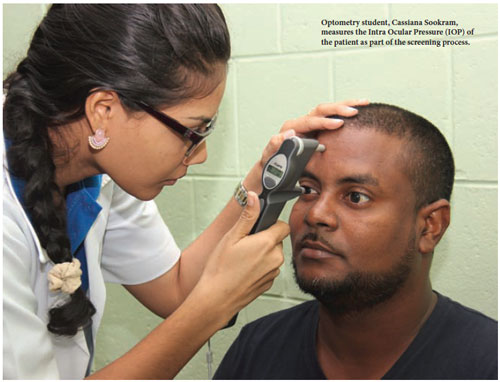
The screening exam, of necessity, consisted of a full history, ophthalmoscopy (examination of the back of the eye or fundus) and the measurement of the patient’s visual acuity and intraocular pressure (IOP).
 Overall, during the 14 hours of screening, we examined 178 patients. This included 13 old glaucoma patients who were being treated and stopped the treatment as their drugs ran out, or who were on a treatment programme, but did not understand what it was all about. These people were counselled, given information on the condition and asked to go back to their clinics to continue their treatment, which was a victory in itself and what primary care is all about. Overall, during the 14 hours of screening, we examined 178 patients. This included 13 old glaucoma patients who were being treated and stopped the treatment as their drugs ran out, or who were on a treatment programme, but did not understand what it was all about. These people were counselled, given information on the condition and asked to go back to their clinics to continue their treatment, which was a victory in itself and what primary care is all about.
During screening we picked up eight (5%) new glaucoma patients who were unaware that they had the condition and we arranged for them to see a specialist for treatment, which was the main aim of the exercise. We also uncovered 18 (10%) suspected patients with ocular hypertension whom we have asked to come in for a more detailed examination and whom we will place on a management programme if they are not confirmed as being glaucomatous.
A third of our patients (60) came from families with confirmed glaucoma, but were unaware that they were likely to develop the condition. This is a very high number and it suggests that education of the population about this devastating disease is sadly lacking and needs to be addressed.
Together these two figures (new and suspected cases, 5% + 10%) add up to 15% of our examined population having or being suspected of having the disease, which conforms to the new, unaudited National Eye Survey of Trinidad and Tobago (NESTT) figures, conducted by UWI Optometry (and others) for the GORTT. If this screening project was not undertaken these people most likely would have gone on to develop glaucoma and would probably have reported for treatment when it was well established, and may have even gone on to lose much of their sight.
Many patients had other conditions as some (46, 25%) didn’t realise that their diabetes had ocular consequences, but knew that their parents had the condition (diabetic-related eye disease). They were advised to see their doctor or go to the local health centre for advice. Others had mature cataracts (11, 0.5%), and were referred to the hospital eye services for consultation while some (19, 10.6%) had early cataracts and were put on a management list for observation at our clinic, or referred to their doctor for further advice.
 There were 11 (6%) patients who were urgently referred to private ophthalmologists or to the hospital eye service for attention, one being a patient with Papillodema, whom we had seen in a screening session previously and asked to return for further examination. This is a very serious condition due to pressure in the cranium which, if not treated immediately, could lead to stroke, blindness and, in very severe cases, to death. There were 11 (6%) patients who were urgently referred to private ophthalmologists or to the hospital eye service for attention, one being a patient with Papillodema, whom we had seen in a screening session previously and asked to return for further examination. This is a very serious condition due to pressure in the cranium which, if not treated immediately, could lead to stroke, blindness and, in very severe cases, to death.
Quite a large number (62, 34.8%) of patients felt they had hazy vision, but left it alone or were unaware that it was caused by a cataract(s) although most had diabetes and hypertension. This is another instance of poor education of the public on eye conditions and must be addressed urgently.
This small project has picked up large numbers of conditions that, if they were not discovered, would go untreated and would have led to unnecessary eye diseases, suffering, loss of many man-hours and production and, ultimately, unemployment, misery and, finally, blindness and death.
Much of this could be avoided by doing ocular screening throughout the country to pick up these conditions early and offer solutions. The Ministry of Health has agreed to make a NESTT bus available for this purpose and we await its arrival anxiously. |





