|
 |
 |
|
April 2014 |
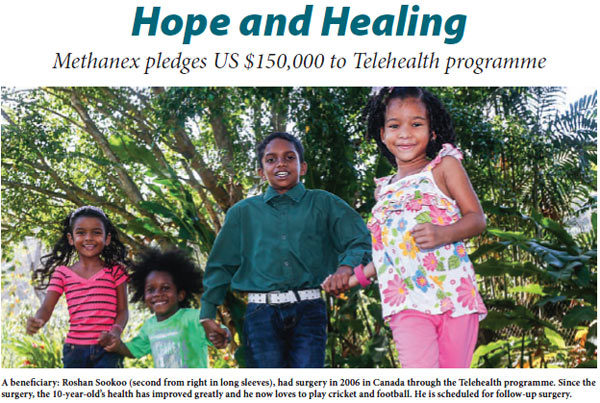
“Brittney was born with congenital heart disease, club finger nails, blood-shot red eyes…she was unable to stand, run or walk for any period of time,” Jitendra Ramai, had his arms around his young daughter while he spoke about her illness a few weeks ago. Like hundreds of others, he is grateful to The UWI Telehealth programme for the hope and healing the initiative gave to Brittney and the family. While reading a UWI publication, Jitendra came across an article that spoke about the programme, which since its launch in 2004, has helped children from 228 families with complicated medical needs – including congenital defects of the bowel, heart, nervous system and other organs, as well as developmental problems such as paediatric cancer and blood disorders – gain access to affordable, quality health care through telecommunications and videoconferencing technology. After surgery in 2008, Brittney’s life changed. Now she can play with her dogs, ride her bike, enjoy a game of football and cricket with her friends. Without it, her Dad said, “Brittney could not have done anything at all. We are so grateful.” The UWI Telehealth programme, with offices located at the Faculty of Medical Sciences, Eric Williams Medical Sciences Complex (EWMSC) at Mt Hope, has benefitted children with complicated medical conditions as well as health care practitioners. Dr. Hilary Lee Cazabon has been integral to the programme since inception. She recently explained that it is a great resource for physicians and surgeons at the Complex who benefit from “consultations, second opinions and possibly referrals” with tertiary institutions abroad. Doctors can also view and learn from medical rounds in other hospitals and in turn share their local experiences and expertise with those abroad. In March, Methanex Trinidad Limited pledged US$150,000 over the next three years in support of the programme. So far, there have been 223 consultations with local and international health care professionals and 19 children have benefitted from free surgeries at The Hospital for Sick Children (SickKids), Canada’s most research-intensive hospital and the largest centre dedicated to improving children's health in Canada. These surgeries have been paid for by the Herbie Fund at an estimated cost of US $1.6 million. The survival rate for those who have benefitted from the programme is 100%. By Anna Walcott Hardy |