|
 |
 |
|
February 2015 |
On June 12, 2014, he presented a paper on “Vector Control Management in the Caribbean region: Lessons ignored” at an event held by CARPHA, the Caribbean Public Health Agency, and CKLN, the Caribbean Knowledge and Learning Network in Port of Spain. He lamented that the same vector control strategies have been used for the past 25 to 30 years without success and it was way past the time to invest in new strategies based on scientific research. He looked at four of the major programmes used regionally, questioning their efficacy under today’s conditions.
Failures in these programmes could be attributed to a series of common factors.
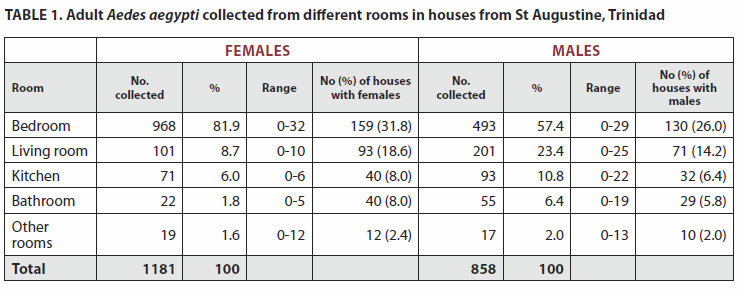
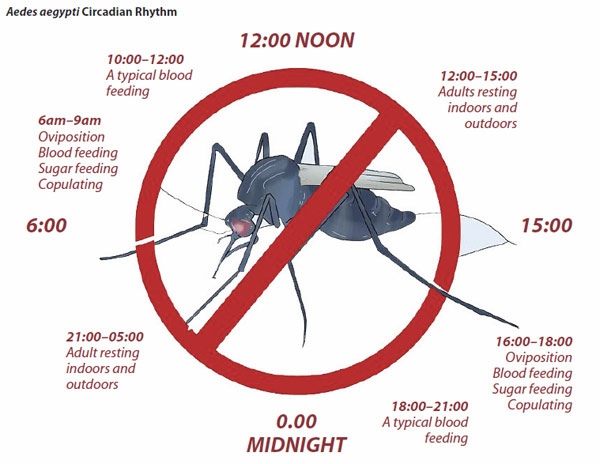
The aerial sprayings, he said, are ineffective because they do not sufficiently penetrate houses to kill the resting mosquitoes. (His research showed that they love to loll off in our bedrooms after a blood meal.) They also negatively affect almost all living things: asthmatics and people with respiratory illnesses; pollinators like butterflies, bees and birds; aquaria fish and chickens on a farm, pigs in piggeries. Generally, the sprays disrupt the functioning of the entire ecosystem; while the mosquitoes keep humming along their merry way. Professor Chadee, who spent many years at the Insect Vector Control Division, has in the past complained that his recommendations for vector control programmes to the Government of the Republic of Trinidad and Tobago have been largely ignored. He offered several suggestion for a different approach to the growing problem of mosquito-driven epidemics. His expertise has been sought in several countries seeking to fight such outbreaks. In the period between 2007 and 2014, he has been to Italy, Brazil, Mauritius, Sri Lanka, the Seychelles, and Reunion Island – there were major outbreaks in the last four. There, “a suite of interventions programmes was developed, including conventional vector control, and with the addition of the Sterile Insect Technology (SIT)” he tells me. SIT is like birth control, he says, sterilizing immature male mosquitoes via radiation and releasing them back into the wild to mate. Since the eggs produced are not viable, the population eventually collapses. It worked in Mauritius and Reunion Island. Although it is expensive, a pilot project is to be implemented in St. Vincent, says Dr James Hospedales, the Executive Director of CARPHA, who has also complained that the “same-old, same-old” strategies of the past few decades are simply not working. “We have to change the vector control paradigms,” he said. “We have to stop the knee-jerk responses. Governments could spray every day and it would not help; the mosquitoes have become resistant.” And it is not vector control that needs different approaches, he says, this Chikungunya virus is a wake-up call to the region. “We have to look at epidemic control too.” “If this were a lethal virus,” he says grimly, “we would be in monkey pants.” He warns that the migratory pattern of the virus shows that it is heading southward and it is here in the region to stay. From 1954 to 2004, Dr Hospedales notes, there were about a million cases of ChikV with outbreaks first in Africa, then South Asia, and Southeast Asia. That is over a fifty-year period. Since the first case of ChikV in the Americas was reported in December 2013 in Saint Martin/Sint Maarten, there are now about a million cases in the region, with 23 of the 24 CARPHA member states affected as at October 27, 2014. Less than one year. As in Dengue and Chikungunya there are similar trajectories, and Dr Hospedales points to a recent one, the Zika virus, which is following the same path and may reasonably be expected to hit the region. It is like Dengue, he says, and may be lethal. Coupled with Professor Chadee’s observation that the Dengue outbreaks had become more frequent over the years, turning up every five years or so, and his prediction that even that will soon become as frequent as every two years; it is of enough gravity to warrant a major shift in public health strategies, because clearly, the mosquitoes are winning these battles. Among the strategies proposed by Professor Chadee, based on research that has been so prolonged and detailed that he has had Dengue twice (along with Dengue Hemorrhagic Fever), are some particularly innovative ones. Based on investigations of several households, his team was able to ascertain that mosquitoes overwhelmingly prefer to rest in bedrooms (81.9%) (see Table 1) and they liked walls best. It explains why DDT was effective when it was applied to walls, and the sprays were not – as they were not as concentrated.
His research on the travelling habits of the mosquitoes revealed two features that he is certain can be applied to stopping them in their tracks. The first is that mosquitoes do not cross highways. “Aedes aegypti mosquitoes, and by extension, the Dengue virus do not cross over highways, so you are ‘genetically’ isolated from either side. So why can’t we use this as part of our control strategy?” He also said that his studies have revealed that mosquitoes do not travel very far, so it would make sense to target the cardinal points in close proximity to infected spaces, instead of broad applications. He even suggested that curtain manufacturers might be persuaded to treat their fabrics with suitable insecticides to help act as barriers to mosquitoes entering homes. It is a novel plan, and one that requires a significant degree of cooperation from the private sector; but an “all-inclusive approach” is also what Dr Hospedales is recommending for the battles ahead. In the complete revamping of strategies, he suggests that there might have to be a return to old techniques such as window-screens, and deployment of new technologies such as mobile phones. “We need more integrated approaches where cellphone companies get involved, for example,” he says, citing Sri Lanka where people are encouraged to send text messages as soon as they feel the onset of symptoms and they are then advised what to do.
Public education is extremely vital to slowing down the progress of any virus, he says. If a person understands that the moment they show signs of the virus, they have to take extra precautions not to be bitten by mosquitoes for at least a week (so as not to further spread the virus), it would help the containment. The consensus is that there is more research to be done – which needs far more funding than any of the Caribbean’s health organisations currently receives – and there is a need for a complete overhaul of the traditional strategies. On March 3 and 4, CARPHA will be part of a consultation bringing together a range of disciplines to discuss Chikungunya, epidemic control and vector control. Private sector organizations and The UWI will be invited as well, and hopefully, soon, a new approach will take shape.
|



 If someone tells you that mosquitoes cannot cross highways and that that might be useful information in preventing their spread, you might blink twice. But if that someone is Dave Chadee, entomologist, parasitologist, and a Professor of Environmental Health at the Department of Life Sciences at The UWI, you might think twice. He is internationally recognized as an expert on mosquitoes and has done a substantial amount of research on the accursed Aedes aegypti mosquito, the carrier of Yellow Fever, Dengue and the Chikungunya virus.
If someone tells you that mosquitoes cannot cross highways and that that might be useful information in preventing their spread, you might blink twice. But if that someone is Dave Chadee, entomologist, parasitologist, and a Professor of Environmental Health at the Department of Life Sciences at The UWI, you might think twice. He is internationally recognized as an expert on mosquitoes and has done a substantial amount of research on the accursed Aedes aegypti mosquito, the carrier of Yellow Fever, Dengue and the Chikungunya virus.