 |
 |
 |
|
March 2013 |
Where did the concept of VBD arise? In the early 1900s, patients needing blood transfusions in England had to find their own blood donors. This practice was deemed inefficient and VBD was initiated in 1921 by Percy Lane Oliver, a Red Cross worker. By 1946, the totally voluntary British National Blood Transfusion Service was established. Nonetheless, replacement blood donation (RBD), whereby patients find their own blood donors to cover an anticipated need or to replace blood used in an emergency, has remained standard practice in many developing countries, notably the English Caribbean. This includes the UWI campus territories of Barbados, Jamaica and Trinidad and Tobago. RBD is often accompanied by paid or remunerated blood donation (PBD) as persons in need may use this method to get others to donate in order to secure medical services. In 1975, WHO advocated blood services based on VBD rather than PBD. PBD were more likely to have infections such as HIV, hepatitis B and syphilis, which could be transmitted by transfusion. This is also the case with RBD. The reason is that persons receiving payment in cash or kind are more likely to conceal aspects of their social life that would ordinarily disqualify them from donating blood. As a result, further resolutions recommending totally VBD and the discontinuation of RBD and PBD have been accepted by WHO member states in the past few decades. PAHO has recommended establishing a network of volunteers to educate the community, promote voluntary blood donation and service blood donors, with special attention to youth programmes. Training health professionals in the clinical use of donated blood is equally important. Member states who have developed services based on 100 % VBD have been shown to collect more blood more safely.
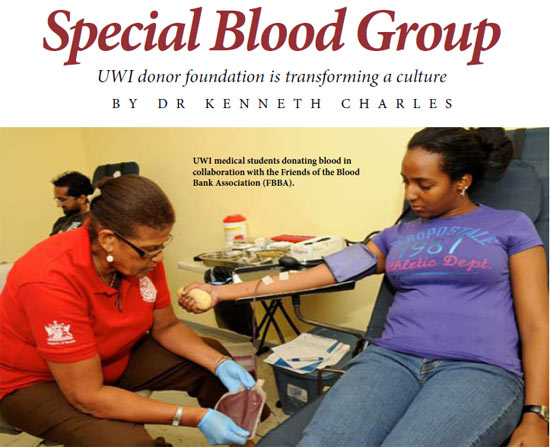
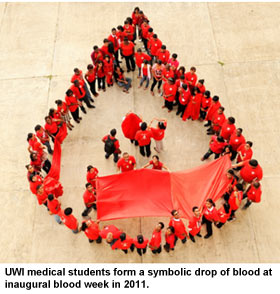
The UWIBDF was founded in 2011 to raise awareness about voluntary blood donation in the community and the efficient use of blood by doctors. It is based at the Department of Paraclinical Sciences (DPS) of the Faculty of Medical Sciences (FMS). Its current members are predominantly voluntary youth organisations, including the Trinidad and Tobago Medical Students Association (TTMSA), the Hindu Students Council (HSC), Share Goodness (SG), the Intervarsity Christian Students’ Fellowship (IVCSF) and the Mount Hope Islamic Society. It has been organising blood drives in collaboration with the Friends of the Blood Bank Association (FBBA), and several research projects on blood donation and use are ongoing at the FMS. The UWIBDF intends to improve blood safety and adequacy using the media of research and education. We believe that this initiative has the potential to contribute to national and regional development in keeping with the University’s strategic plan 2012-2017. -Dr Kenneth Charles is a Senior Lecturer at the Department of Paraclinical Sciences, Faculty of Medical Sciences, UWI, St. Augustine. This is adapted from a presentation he made at the Conference hosted by FMS: “Improvement in Health Care Quality and Devlivery: Making a Difference” in January 2013. Photography courtesy Dr Kenneth Charles. |

 Raising public awareness could increase voluntary blood donation and impact health care delivery in Trinidad and Tobago. A safe and reliable blood supply which is donated unconditionally and anonymously and used on a basis of clinical need would address the country’s needs – emergencies, planned surgeries, pregnancy complications, dialysis, oncology and haematology. It would improve the lives of patients who require repeated blood transfusions to stay alive and those, including foreign visitors, who have no relatives to donate blood on their behalf. It was out of this knowledge that the University of the West Indies Blood Donor Foundation (UWIBDF) was born.
Raising public awareness could increase voluntary blood donation and impact health care delivery in Trinidad and Tobago. A safe and reliable blood supply which is donated unconditionally and anonymously and used on a basis of clinical need would address the country’s needs – emergencies, planned surgeries, pregnancy complications, dialysis, oncology and haematology. It would improve the lives of patients who require repeated blood transfusions to stay alive and those, including foreign visitors, who have no relatives to donate blood on their behalf. It was out of this knowledge that the University of the West Indies Blood Donor Foundation (UWIBDF) was born.